Informed consent in aesthetic surgery is more than just signing a form - it's a detailed process that ensures patients fully understand the procedure, risks, benefits, and alternatives. This approach protects both patients and providers, fostering trust and better outcomes. Here's what you need to know:
- What it is: Patients receive clear, honest information about the procedure, including risks, benefits, and alternatives.
- Why it matters: Aesthetic surgeries are elective, making informed decisions and patient autonomy critical.
- Key elements: Clear communication, proper documentation, and tailored discussions for specific procedures.
- Legal and ethical standards: Providers must meet federal and state laws while respecting patient autonomy.
- Digital tools: Platforms like Prospyr simplify consent management, ensuring accuracy, security, and compliance.
The process emphasizes patient understanding, realistic expectations, and shared decision-making, creating a safer and more transparent experience for everyone involved.
Dr. Lara Wetton - Informed Consent in Cosmetic Surgery
Core Elements of a Valid Informed Consent Process
A proper informed consent process is built on critical components that ensure patients can make well-informed decisions about their aesthetic procedures. Each element serves a specific purpose, helping patients understand risks, benefits, and alternatives.
Required Information in Consent Forms
An effective consent form must include several key details to meet both ethical and legal standards. To start, it should clearly describe the procedure in straightforward, easy-to-understand language. Patients should know exactly what will happen during surgery.
The form should also outline potential risks, covering both common and rare complications. For example, risks like infection, scarring, asymmetry, and dissatisfaction with results should be addressed. For procedures like breast augmentation, it’s important to mention specific risks such as implant rupture or the possibility of needing revision surgeries.
The benefits section should present realistic expectations. Instead of promising "perfect results", it should explain typical improvements while acknowledging that outcomes can vary based on individual healing and other factors.
Patients should also be informed about all available options, including nonsurgical alternatives and the choice to avoid treatment altogether. For instance, someone considering facial rejuvenation might weigh the pros and cons of a surgical facelift versus non-invasive options like dermal fillers or laser treatments.
Costs need to be transparent. The form should break down all fees, such as surgeon, facility, and anesthesia costs, as well as potential additional expenses if complications arise or further procedures are required.
Lastly, the recovery timeline should set clear expectations. Patients need to know how long downtime will last, when they can return to work or exercise, and what signs might indicate the need for immediate medical attention. These details are crucial for informed decision-making.
Special Considerations for Different Patient Groups
Certain patient groups require extra care during the consent process. For minors, additional safeguards are necessary. Written consent from both parents or legal guardians is typically required, and in some cases, a psychological evaluation may be recommended. Organizations like the American Society of Plastic Surgeons often advise waiting until physical maturity is reached before undergoing elective procedures.
For non-English speaking patients, consent forms should be translated into their primary language. Using qualified medical interpreters during consultations is essential to ensure accurate communication. Family members should not serve as interpreters, as this can lead to conflicts of interest or miscommunication. Any modifications made for these patients should be documented to ensure compliance with legal standards.
Patients with cognitive impairments or mental health conditions may need a tailored consent process. Providers should assess these patients' ability to make decisions and involve family members, legal guardians, or mental health professionals when appropriate. Simplified explanations or extended consultations can help ensure understanding.
Special care is also critical for patients with body dysmorphic disorder. These individuals may have unrealistic expectations or seek unnecessary procedures. Screening tools or psychological evaluations can help identify patients who may not be suitable candidates for elective surgery.
Documentation and Compliance Standards
Thorough documentation is essential to complete the informed consent process. Detailed notes from consultations should capture the patient’s questions, concerns, and understanding of the procedure. These records demonstrate that meaningful discussions took place and that the patient was actively involved in the decision-making process.
Having a witness present during the consent discussion and signature process - especially for complex or high-risk procedures - adds another layer of protection. This ensures proper procedures were followed.
Timing is another crucial factor. Patients should ideally receive and sign consent forms well before the procedure, not on the day of surgery (except in emergencies). Providing forms during the initial consultation allows time for review and questions, with final confirmation at a pre-operative appointment.
Digital signatures are acceptable when properly secured. Electronic systems can prompt patients to acknowledge key points and flag incomplete sections, ensuring nothing is overlooked.
Finally, consent documents must be stored securely and retained according to regulatory requirements. Most states mandate keeping these records for at least seven years after the procedure. Digital storage systems should include strong security measures and backup protocols to protect patient privacy while ensuring long-term access.
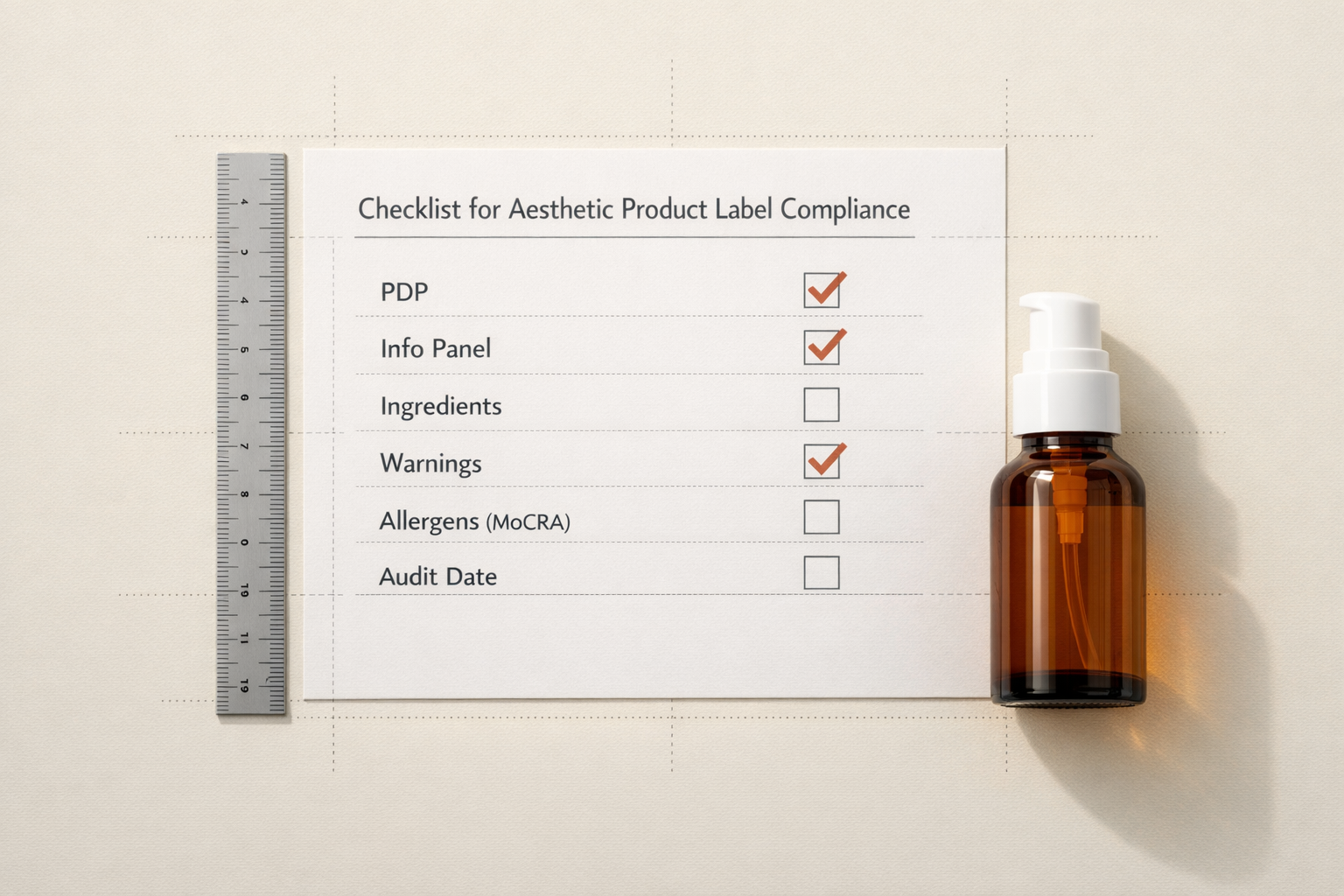
It’s also important to manage version control for consent forms. Each form should include a version date, and practices must ensure that only the most up-to-date version is used. Relying on outdated forms can lead to legal risks if they don’t reflect current standards or known risks.
Best Practices for Procedure-Specific Consent in Surgical Aesthetics
General consent forms are a starting point, but when it comes to surgical aesthetics, personalized discussions are crucial. Each procedure carries its own set of risks and benefits, which need to be clearly communicated to patients. A generic, one-size-fits-all approach simply won’t cut it, especially given the wide range of procedures - from minor enhancements to intricate reconstructive surgeries.
Procedure-Specific Risks and Benefits
Informed consent isn’t just about covering the basics. It’s about tailoring the conversation to the specific procedure at hand.
- Rhinoplasty: Highlight the complexity of the surgery and potential challenges like breathing difficulties or the need for revision surgery. Explain that perfect symmetry may not be achievable due to natural facial asymmetry, and emphasize that the final results take time to fully emerge.
- Breast Augmentation: Discuss implant-specific risks, including the fact that implants aren’t lifetime devices. Patients should be aware of the need for ongoing monitoring and the possibility of future procedures to maintain their results.
- Facelifts: Address the risk of nerve injury and the possibility of scarring that may heal unpredictably. While incisions are generally designed to be discreet, individual healing variations can affect how scars appear.
- Tummy Tucks: Be upfront about permanent scarring, strict recovery protocols, and potential healing complications. Also, advise patients that future changes to their body, such as weight fluctuations, could alter the results.
- Brazilian Butt Lifts: Clearly explain the rare but serious complications associated with the procedure and stress the importance of rigorous post-operative care.
Elective vs. Medically Necessary Procedures
It’s important to differentiate between elective cosmetic procedures and those deemed medically necessary. For elective surgeries, discuss all available alternatives, including the option of non-intervention. On the other hand, reconstructive procedures that address medical concerns should balance functional needs with aesthetic goals. For surgeries that combine both cosmetic and medical elements, clarify which aspects are medically necessary and how that might affect insurance coverage. Additionally, exploring the psychological motivations behind elective procedures can help patients set realistic expectations.
Cooling-Off Periods for Patient Reflection
Allowing patients time to reflect can greatly enhance the consent process. Introducing a cooling-off period gives them the chance to review information, seek second opinions, and weigh their options outside the clinical setting. A staged consent process can be particularly effective - patients provide initial agreement during the consultation and then reconfirm their decision closer to the surgery date. This approach ensures they have ample time to address any lingering questions or concerns.
Effective Communication and Shared Decision-Making
Effective communication takes the consent process beyond just explaining procedures - it turns it into a true partnership. Informed consent isn’t just about delivering information; it’s about creating a dialogue. When patients feel heard and actively involved in decision-making, they tend to have more realistic expectations and better experiences. This approach shifts consent from being a mere formality to a meaningful collaboration between the patient and provider.
Shared Decision-Making in Aesthetic Surgery
Clear communication plays a crucial role in building trust and making sound decisions, particularly in elective surgeries that impact appearance and self-image. Shared decision-making transforms the patient-provider relationship into a collaborative effort.
It all starts with active listening. When patients describe their aesthetic goals, providers should dig deeper to understand the motivations behind them. For example, a patient asking for a rhinoplasty might say they want a "smaller nose", but further discussion could reveal concerns about facial balance or breathing issues. By uncovering these underlying concerns, providers can better address the patient’s needs and manage expectations.
Transparency in presenting options is equally critical. Instead of steering patients toward a specific procedure, providers should outline all viable approaches, including non-surgical alternatives or even delaying treatment. For instance, someone considering a facelift might benefit from learning about injectable treatments, skin resurfacing, or thread lifts, along with their respective risks and recovery times.
Acknowledging uncertainty is another key element. Aesthetic results can vary widely between patients, and being upfront about this variability builds trust. When providers openly discuss the unpredictability of individual healing patterns or the limits of certain procedures, patients are better equipped to make informed choices.
This collaborative model naturally leads to methods that ensure patients fully understand what they’re agreeing to.
Techniques to Ensure Patient Understanding
Helping patients understand goes far beyond handing them a brochure or reading aloud. Skilled providers use a mix of strategies to confirm comprehension.
The teach-back method is particularly effective. After explaining a procedure’s risks and benefits, ask the patient to repeat the information in their own words. This ensures they’ve grasped the key points. Visual aids, like before-and-after photos, can also help clarify complex concepts. However, these tools should set realistic expectations rather than showcasing only the best outcomes. Providers should also explain how factors like skin type, age, or healing tendencies might influence results.
Analogies and simplified explanations are great for breaking down medical jargon. For instance, when describing fat grafting, comparing it to "moving soil from one part of a garden to another" helps patients understand that not all transferred material will "take" in the new location. These comparisons should be straightforward and accurate.
Written summaries complement verbal discussions by giving patients something to review later. These should be in plain language, avoiding heavy medical terminology. Include essential details like recovery timelines, activity restrictions, and warning signs that might require immediate attention.
Communication Strategies for Diverse Patient Needs
Effective communication must adapt to the varied needs of patients, including differences in language, literacy, cultural background, and emotional state.
Language barriers require more than quick translations. Professional interpreters and consent forms in the patient’s primary language are essential for clear communication. On-the-spot translations should only supplement, not replace, fully prepared materials.
Health literacy levels can vary widely. Some patients come well-informed, while others may struggle with basic concepts. Providers should assess each patient’s understanding early and tailor their communication style accordingly. For those with limited health literacy, focus on the most critical points, use simple language, and confirm understanding throughout the conversation.
Cultural factors often influence how patients approach medical decisions. Some cultures prioritize family involvement, while others emphasize individual choice. Age, gender, and religious beliefs can also shape perspectives on aesthetic procedures and their risks. Providers should remain sensitive to these influences while ensuring the patient themselves understands and consents to the treatment.
Emotional states, such as anxiety, can make it hard for patients to process information. If a patient seems overwhelmed, consider scheduling a follow-up consultation. This break allows them to process the information and make a decision with a clear mind.
Technology preferences also play a role. While some patients prefer digital presentations and online resources, others might feel more comfortable with printed materials they can review and annotate. Offering information in multiple formats ensures accessibility for everyone, regardless of their comfort with technology. This approach ties into the documentation and digital management strategies discussed in the next section.
sbb-itb-02f5876
Digital Consent Management and Regulatory Compliance
The move toward digital consent management has reshaped how aesthetic surgery practices handle informed consent. Modern digital platforms bring a host of advantages over old-fashioned paper-based systems, especially when it comes to security, efficiency, and staying compliant with regulations. By building on strong documentation practices, these tools improve both patient care and adherence to regulatory standards.
Benefits of Digital Consent Tools
Digital consent platforms solve many of the headaches that come with paper-based systems. For instance, retrieving consent documents becomes a breeze - if a patient calls months after their procedure with questions, staff can instantly pull up the necessary forms without sifting through physical files.
These platforms also ensure that forms stay up-to-date. Real-time updates mean practices can replace outdated consent forms with the latest versions, keeping in line with new procedures or updated recovery guidelines. This reduces the chance of using forms that miss critical details.
Another major perk is accessibility. Patients can review consent forms at home, giving them the time to fully understand the information and even share it with family or advisors. This leads to better-informed decisions. Plus, practices save on printing and storage costs while avoiding risks like misplaced or damaged documents.
Digital consent tools also integrate seamlessly with patient records, scheduling, and billing systems. This connectivity ensures that a patient’s consent status is always accurately reflected in their digital chart, making operations smoother and ensuring compliance without extra manual steps.
Features of Prospyr for Consent Management

Prospyr’s practice management platform takes digital consent to the next level for aesthetic surgery practices. With its built-in CRM/EMR integration, Prospyr’s digital intake forms automatically fill in patient details, cutting down on data entry errors and saving time during consultations. These forms go beyond basic consent, capturing key information such as medical history and aesthetic goals, which then flows directly into the patient’s record.
Prospyr also prioritizes security with its HIPAA-compliant infrastructure, ensuring that all consent documentation meets strict privacy and security standards. This secure integration not only helps practices stay compliant but also boosts overall efficiency. It’s a clear upgrade from traditional paper-based methods.
Paper vs. Digital Consent: A Comparison
Here’s a closer look at how paper and digital consent methods stack up:
| Aspect | Paper Consent | Digital Consent |
|---|---|---|
| Storage Requirements | Bulky filing cabinets, sometimes off-site | Cloud-based storage requiring minimal space |
| Retrieval Time | 5–15 minutes searching through files | Instant access with a quick search |
| Version Control | Manual updates prone to errors | Automatic updates to ensure accuracy |
| Patient Access | Requires visiting the office | Available 24/7 on any device |
| Backup Security | Vulnerable to damage or theft | Encrypted backups for added security |
| Compliance Tracking | Manual checks | Automated reporting for easy audits |
| Integration | Manual data entry | Smooth EMR integration |
| Cost per Document | $2–$5 (printing and storage) | $0.10–$0.50 per form |
Digital systems also log every access and retrieval, offering a level of accountability that paper records simply can’t match. Automated compliance features make it easy to generate reports for audits or accreditation, saving time and reducing stress.
Switching to digital consent management isn’t just about adopting new technology - it’s a strategic move that improves patient communication, simplifies regulatory compliance, and streamlines practice operations. These tools tie together patient understanding, accurate documentation, and adherence to regulations, creating a more efficient and patient-centered approach. As aesthetic surgery continues to evolve, practices that embrace digital tools will be better equipped to deliver superior outcomes and smoother workflows.
Conclusion and Key Takeaways
Informed consent is the cornerstone of ethical and safe practice in aesthetic surgery. It not only safeguards both patients and providers but also fosters trust, paving the way for better outcomes.
Summary of Best Practices
The most effective informed consent processes share a few common elements. First, consent forms should clearly outline the specific risks, benefits, alternatives, and potential outcomes of a procedure in straightforward, easy-to-understand language. Avoiding overly technical medical terms and breaking down complex concepts ensures patients fully grasp what’s being communicated.
Equally important is patient-centered communication. The best practices create an environment where patients feel at ease to ask questions and voice concerns. Understanding that patients absorb information differently - whether through written materials, visual aids, or personal discussions - can significantly enhance their comprehension.
Allowing a "cooling-off" period is another essential component. This gives patients time to reflect on their decision, reducing the likelihood of regret and boosting their overall satisfaction with the process.
These strategies align with the communication and documentation principles discussed earlier, ensuring a more thorough and patient-focused consent process.
The Role of Technology in Streamlining Consent
In addition to clinical best practices, digital tools are playing an increasingly important role in improving the consent process. Platforms like Prospyr illustrate how technology can simplify and enhance informed consent procedures.
Digital systems help streamline tasks like data entry, automatically update forms, and securely store records, all of which improve compliance. For example, Prospyr’s digital intake forms allow patient information to flow seamlessly across all relevant documents, reducing errors and saving time. When a patient updates their medical history or contact details, these changes are automatically reflected in all necessary forms - no manual input required.
Another advantage of digital tools is that they enable patients to review consent materials at home. This gives them time to process the information and come back with more informed questions, fostering a collaborative approach and setting realistic expectations.
The move toward digital consent management is a smart investment in patient safety, regulatory compliance, and operational efficiency. As aesthetic surgery continues to advance, practices that integrate these tools will be better equipped to provide exceptional care while maintaining the highest standards of informed consent.
FAQs
How can patients make sure they fully understand the informed consent process before having aesthetic surgery?
Understanding the Informed Consent Process for Aesthetic Surgery
Before committing to aesthetic surgery, it’s crucial to have a clear grasp of the informed consent process. Start by asking your surgeon to provide a detailed explanation of the procedure. This might involve verbal discussions, written handouts, or even visual aids like diagrams to help clarify complex concepts. Be proactive - ask specific questions about the risks, potential benefits, and any alternative treatments. Make sure the information is shared in a way that’s easy for you to understand.
Take your time reviewing the consent form. Double-check that all the details are accurate and nothing feels unclear. Only sign the form once every question you have is answered and you feel fully confident in your understanding of the procedure and what it entails. These steps will help you make a well-informed decision about your care. Confidence comes from clarity, so don’t rush the process.
How can digital tools like Prospyr improve the informed consent process in aesthetic surgery?
Digital platforms like Prospyr are transforming the informed consent process in aesthetic surgery, making it more efficient and user-friendly for both patients and providers. With Prospyr, practices can design, tailor, and securely store consent forms while staying aligned with the latest regulatory requirements. The addition of electronic signatures eliminates the hassle of excessive paperwork and provides a dependable audit trail, ensuring accuracy and legal security.
Beyond operational convenience, these tools elevate the patient experience. Patients can access, review, and sign consent forms directly from their devices, offering them the flexibility to fully understand the information at their own pace. This digital approach not only boosts patient engagement but also simplifies the entire process. By streamlining these essential tasks, Prospyr allows practices to save time, maintain precision, and present a polished, professional experience for everyone involved.
Why is a cooling-off period recommended before confirming consent for cosmetic surgery?
The Importance of a Cooling-Off Period for Cosmetic Surgery
A cooling-off period is an essential step before finalizing consent for cosmetic surgery. It gives patients the opportunity to carefully think through their decision, seek out more information, and discuss their plans with trusted friends, family, or advisors. This pause ensures that the choice to proceed is both deliberate and fully informed.
Typically ranging from 7 to 14 days, this period is designed to prevent hasty decisions that might lead to regret or dissatisfaction later on. By taking this time, patients can approach their procedure with confidence and readiness, putting their safety and long-term happiness at the forefront.