Telehealth reimbursement can be challenging, but staying compliant ensures your clinic avoids claim denials, audits, or repayment demands. Here's what you need to know:
- Licensure: Providers must be licensed in the state where the patient is located during the visit. Verify licenses monthly and log details like expiration dates and multistate privileges.
- Payer Policies: Medicare, Medicaid, and private insurers have unique telehealth rules. Review covered codes, eligible provider types, and payment terms for each.
- Billing Accuracy: Use correct CPT/HCPCS codes, modifiers (e.g., 95, GT), and place-of-service codes (e.g., POS 02 or 10). Document visits thoroughly, including consent, locations, modality, and medical necessity.
- Technology: Use HIPAA-compliant platforms that integrate with your EHR and streamline scheduling, billing, and documentation.
- Staff Training: Train your team regularly on telehealth policies, coding practices, and payer updates.
- Audits: Conduct quarterly audits to identify gaps in compliance and improve workflows.
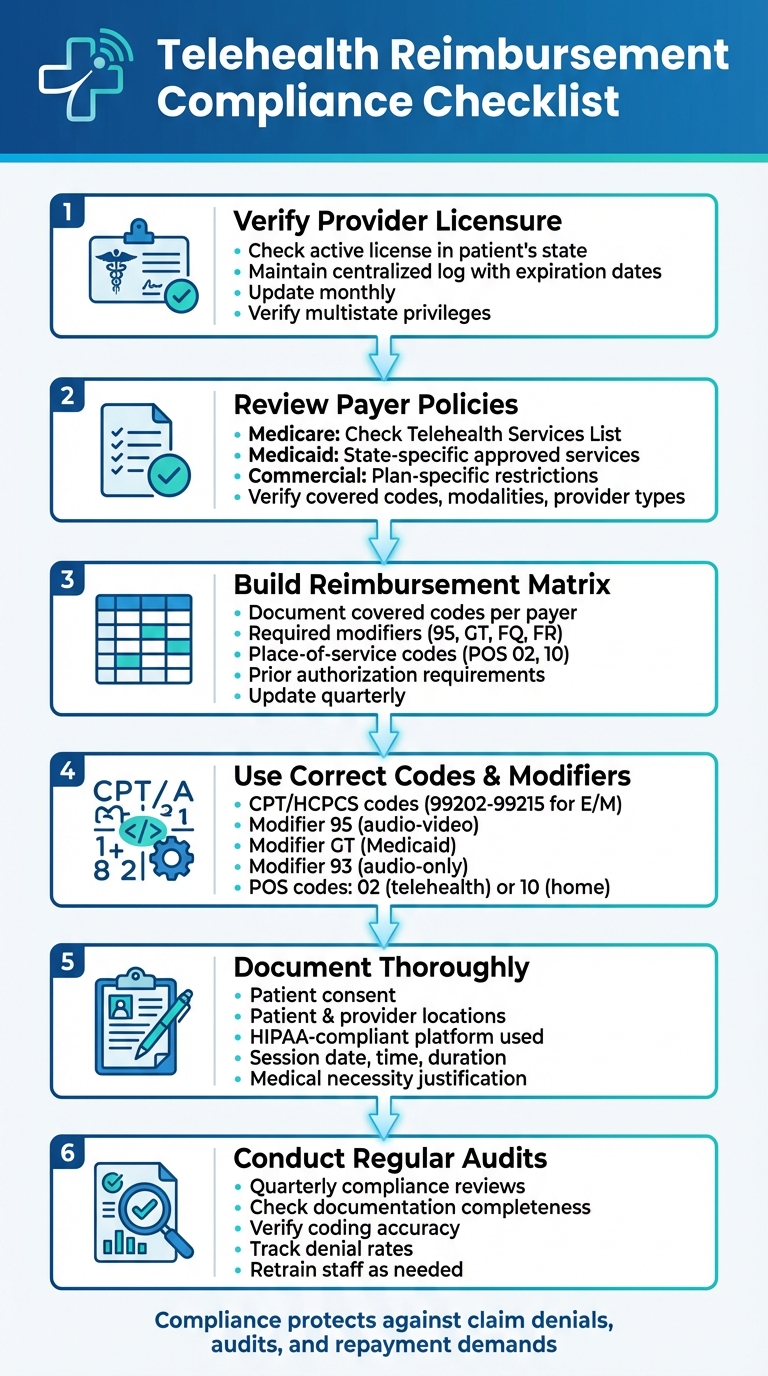
Telehealth Reimbursement Compliance Checklist: 6 Essential Steps
Regulatory and Policy Requirements
Before billing for telehealth services, you need to confirm three key elements: provider licensure, payer policies, and an internal reimbursement matrix. Missing any of these steps can result in denied claims, repayment demands, or even regulatory scrutiny. These checks are the backbone of accurate billing and thorough documentation.
Check Provider Licensure and Practice Scope
Providers must have an active license in the state where the patient is located at the time of the visit. If a patient moves, you’ll need to verify licensure for each appointment. Some states offer specific telehealth licenses, interstate compacts (like the Interstate Medical Licensure Compact for physicians or the Nurse Licensure Compact for RNs), or temporary practice exceptions, but these vary widely and require state-by-state verification.
Beyond licensure, the provider’s scope of practice also comes into play. State laws dictate what services different providers - physicians, nurse practitioners (NPs), physician assistants (PAs), registered dietitians - can perform via telehealth. For example, some states impose stricter limits on NPs and PAs, particularly for prescribing weight-management medications or conducting certain aesthetic consultations.
To stay organized, maintain a centralized log with each provider’s license number, issuing state, expiration date, and any multistate privileges. Update this log at least monthly. When scheduling out-of-state patients, cross-check the log and consult your compliance or legal team if there are uncertainties.
Review Payer Telehealth Policies
Telehealth reimbursement rules differ across Medicare, Medicaid, and commercial insurers. Medicare, for instance, outlines covered telehealth services in its official Telehealth Services List. It also specifies eligible provider types (e.g., physicians, nurse practitioners, clinical psychologists) and sets rules on patient location and delivery methods. These policies are evolving, especially as COVID-era flexibilities are set to expire in late 2025.
Medicaid coverage varies by state. Each state’s Medicaid program publishes its own list of approved telehealth services, allowed modalities (like two-way video, audio-only, or remote monitoring), and eligible provider types. Commercial insurers, on the other hand, follow state telehealth mandates and their internal policies. These may include plan-specific restrictions on patient locations, modalities, and provider networks.
For every payer, it’s crucial to review these details:
- Covered telehealth CPT/HCPCS codes
- Allowed modalities
- Eligible provider types
- Geographic and originating site rules
- Payment terms, including whether telehealth is reimbursed at the same rate as in-person visits (payment parity) or at reduced rates.
Organize these details into easy-to-access payer fact sheets for your team.
Build a Telehealth Reimbursement Matrix
A reimbursement matrix simplifies billing by consolidating all payer-specific telehealth requirements. For each payer, include:
- Covered telehealth codes
- Required modifiers (e.g., 95, GT, FQ, or FR)
- Correct place-of-service codes
- Allowed modalities
- Prior authorization requirements
- Rate details or parity notes.
Tailor the matrix to your clinic’s services, flagging codes for virtual consultations, follow-ups, weight-management counseling, behavioral health sessions, and remote monitoring. Note any frequency limits or time thresholds.
Make sure the matrix includes effective dates for temporary or expiring flexibilities so staff can adjust coding practices as needed. Assign a compliance lead to update the matrix quarterly, referencing reliable sources. Regular internal audits of denied claims and payer notices can help identify compliance gaps, prompting updates and staff retraining.
Using a HIPAA-compliant platform like Prospyr can streamline this process. These platforms integrate payer-specific telehealth rules into scheduling and billing workflows, automatically capture key data (e.g., patient location, modality, and consent), and offer analytics to track telehealth denials and revenue trends by payer.
Billing and Documentation Requirements
After regulatory verification, ensuring accurate coding and thorough documentation is key to securing telehealth reimbursements. Even a small oversight, like a missing modifier or incomplete note, can lead to claim denials.
Use Correct Codes and Modifiers
Choosing the right CPT/HCPCS code is crucial for every service. In aesthetic and wellness clinics, most virtual visits are billed using evaluation and management (E/M) codes for new or established patients (e.g., 99202–99215) when conducted via synchronous audio-video. Brief virtual check-ins may use code G2012, while remote image evaluations might require G2010, depending on the situation. To simplify this process, create and update a code reference guide annually. This guide should map common services - like cosmetic consultations, pre- and post-procedure reviews, and weight-management check-ins - to the correct codes, aligning with the latest CMS guidance and major commercial payer updates.
Modifiers play an equally important role. Use 95 for synchronous audio-video visits, GT for certain Medicaid cases, and 93 for audio-only visits when permitted. Pair these modifiers with the appropriate place-of-service (POS) code. For example, use POS 02 for telehealth visits conducted outside the patient’s home and POS 10 for home-based telehealth visits. In some cases, like specific state Medicaid programs, you may need to combine in-person POS codes (e.g., 11 for an office visit) with modifiers like 95 or GT. To minimize errors, integrate payer-specific coding rules into your practice management system.
Document Telehealth Encounters Completely
Every telehealth note must fully support the billed codes to pass audits. Key elements to include are:
- Patient consent: For example, "Verbal consent for telehealth obtained on 03/10/2025."
- Patient’s location at the time of the visit.
- Provider’s location during the session.
- Telehealth modality and the HIPAA-compliant platform used.
- Session details: Date, start and stop times, and total duration for time-based codes.
Clinical notes should comprehensively address the chief complaint, medical history, exam findings (such as visual inspections for injection sites, skin irritation, or swelling), assessment, and treatment plan. For wellness or weight-management programs, include specific diagnoses like obesity, PCOS, or metabolic syndrome, as well as risk factors and counseling details. This helps distinguish between covered medical care and elective or cosmetic services. Be sure to document any orders, prescriptions, or referrals, along with clear follow-up instructions. Using standardized EHR templates can help ensure no critical details are missed. Platforms like Prospyr can also automate the capture of key billing fields, embedding compliance directly into your workflow.
Confirm Coverage and Get Prior Authorizations
Once documentation is complete, the next step is verifying coverage and securing any required pre-authorizations to avoid claim denials. Confirm telehealth benefits, including service coverage, allowed modalities, and any restrictions, before scheduling appointments. Automated prompts in your practice management system can ensure active coverage and patient consent are verified before claims are prepared or appointments checked in.
For services requiring prior authorization, make sure to clearly label the visit as telehealth. Document all payer details, including required codes, clinical data (e.g., photos, lab results, or BMI trends), authorization numbers, approval or denial dates, and visit limits. Include the payer’s name, contact method, reference numbers, and other essential details in the EHR. Attach scanned authorization letters or screenshots when possible. Linking prior authorization statuses to scheduling and billing workflows helps prevent claims from being submitted prematurely, reducing denials and unnecessary write-offs.
Technology and Operations Setup
Accurate billing is just one part of the puzzle. To complete your compliance framework, you need solid technology and efficient operations. Even the most precise coding won’t guarantee reimbursement without a secure platform and a well-prepared team.
Use HIPAA-Compliant Telehealth Platforms
Your telehealth platform must meet HIPAA standards to ensure secure data transmission, proper access controls, and comprehensive audit logs. It’s also essential that your vendor signs a Business Associate Agreement (BAA) outlining their responsibility for protecting patient information and reporting any breaches. Keep in mind, the U.S. Department of Health and Human Services (HHS) now requires healthcare providers to use platforms specifically designed for medical use - consumer video tools allowed during the COVID-19 emergency no longer meet the requirements.
For aesthetic and wellness clinics, prioritize platforms that integrate smoothly with your existing EHR or CRM systems. Look for features like secure image and file sharing, automatic capture of billing data (e.g., session time, patient and provider locations, visit modality), and easy documentation. Solutions like Prospyr offer an all-in-one, HIPAA-compliant platform that combines telehealth, scheduling, documentation, payment processing, and communication tools.
Train Staff on Telehealth Billing
Your team’s training is just as important as having the right technology. Conduct annual training sessions for all front-desk, clinical, and billing staff, with quarterly updates to keep everyone informed about the latest policies and coding practices. Use real-world claim examples to make the training practical and relatable, and designate a telehealth champion to stay on top of policy changes.
Front-desk and scheduling staff should be equipped to verify telehealth coverage before scheduling appointments, confirm patient locations, and understand when an in-person visit is required due to payer or licensing rules. They should also document key details like consent, session time, and modality while ensuring accuracy with modifiers and place-of-service codes.
To make training manageable, consider short webinars, quick-reference tip sheets, and hands-on coding exercises. These tools can keep your team up to date without overwhelming them.
Run Regular Compliance Audits
Regular audits are essential for maintaining compliance and addressing issues before they hurt your bottom line. Quarterly audits can help you verify that telehealth encounters meet all necessary requirements, from proper documentation to accurate coding.
For each audited visit, check that the records include patient consent, correct patient and provider locations, the appropriate visit modality (audio or video), and all clinical details that justify the medical necessity of the service. Ensure that the CPT/HCPCS codes match those listed on CMS’s Telehealth Services List or your state Medicaid’s approved list, and confirm that modifiers and place-of-service codes align with payer guidelines.
Practice analytics tools, like those offered by Prospyr, can simplify this process by tracking metrics such as claim denial rates and missing documentation. These insights allow you to spot and fix problems early, protecting your revenue and ensuring compliance.
sbb-itb-02f5876
Telehealth Applications for Aesthetic and Wellness Clinics
Virtual Consultations and Follow-Up Visits
When it comes to telehealth reimbursement, distinguishing between medical and cosmetic services is crucial. Virtual consultations addressing medical conditions like acne, rosacea, dermatitis, or post-procedure wound care often qualify for reimbursement, as these involve diagnosable conditions with health implications. On the other hand, purely cosmetic discussions - such as planning Botox treatments for aesthetic purposes or exploring filler options - are typically self-pay, as they don’t meet the standards for medical necessity.
To ensure reimbursement, proper documentation is key. Many clinics use standardized telehealth templates with fields like “Visit Purpose: Medical vs. Cosmetic” and “Medical Necessity Rationale” to clearly outline why a visit is billed to insurance rather than categorized as an elective service. For follow-up visits, it’s important to separate billable medical reviews from cosmetic discussions. By documenting medical aspects thoroughly and noting cosmetic elements as self-pay, clinics can maintain clear service categorization and accurate billing practices.
Weight Management and Wellness Programs
Telehealth weight management programs, when structured properly, can be a strong source of reimbursable services. Medicare and many commercial insurers cover virtual visits for obesity counseling, nutrition therapy, diabetes prevention, and chronic disease management. To qualify, specific criteria must be met, such as documented BMI thresholds, appropriate ICD-10 codes (e.g., E66.x for obesity), and evidence-based counseling tied to conditions like prediabetes or hypertension.
Remote monitoring options can further boost revenue. For example, Remote Patient Monitoring (RPM) for tracking blood pressure or weight and Remote Therapeutic Monitoring (RTM) for exercise or medication adherence are reimbursable, provided CPT-defined thresholds are met. This includes using FDA-cleared devices and meeting data collection requirements. Medicare’s CCM code 99490 reimburses approximately $60.49 for 20 minutes of care, with an additional 20 minutes billed under code 99439 for about $45.93.
Before launching a telehealth wellness program, it’s essential to confirm payer-specific requirements. This includes verifying necessary CPT/HCPCS codes and modifiers, understanding whether audio-only visits are allowed, checking visit frequency limits, and determining if in-person initiation or periodic follow-ups are required. Detailed documentation - such as the patient’s BMI, comorbidities, counseling provided, time spent, and treatment goals - is critical for compliance with payer standards.
Simplify Compliance with Prospyr

Technology can make telehealth compliance more manageable. Prospyr offers tools that streamline workflows and ensure adherence to reimbursement guidelines. For instance, Prospyr’s digital intake forms collect telehealth consent, chief complaints, medications, and relevant history upfront, automatically funneling cosmetic requests to self-pay while billing medical concerns correctly. Its integrated scheduling system allows staff to tag appointments as telehealth and specify the type of visit - whether medical, cosmetic, weight management, or post-procedure follow-up - ensuring the right templates and billing rules are applied.
Prospyr also integrates with EMR/CRM systems, using AI-powered note creation to embed compliance details into records. This includes patient and provider locations, telehealth modality (video or audio-only), time spent, and documentation supporting medical necessity. Additionally, its payment and membership management tools separate reimbursable services from self-pay cosmetic packages, minimizing the risk of billing errors. Prospyr’s practice analytics further provide insights into telehealth utilization, denial trends, and payer mix, helping clinics adapt as CMS and payer policies change.
Conclusion
Keeping up with telehealth reimbursement compliance requires ongoing effort and attention to detail. Start by embedding compliance into your daily workflows: verify licensure, maintain a reimbursement matrix tailored to each payer, and ensure the use of accurate codes with the correct modifiers. Solid documentation is key - this includes noting consent, patient and provider locations, modality (audio or video), time spent, and medical necessity. These steps can help shield your clinic from claim denials and audits.
To strengthen your compliance strategy, designate an internal compliance lead to stay on top of updates from CMS, HHS, and individual payers. Conduct quarterly reviews of your telehealth policies, perform internal audits on a sample of charts and claims, and offer targeted training for schedulers, providers, and billing staff. This proactive approach helps identify and address documentation gaps early. Track metrics like claim denial rates and documentation accuracy to gauge the effectiveness of your efforts.
Leverage technology to simplify the process. A HIPAA-compliant platform like Prospyr can centralize scheduling, billing, and documentation. Prospyr’s built-in templates include fields for essential details - such as consent, modality, locations, and time - ensuring that compliance information is consistently captured. Its AI-powered tools can identify trends in claim denials by payer or service type, allowing you to address issues before they escalate.
Make compliance a seamless part of your operations. Hold a team review to identify immediate improvements, implement quick fixes, and establish a plan for ongoing updates. Start by auditing recent claims, then set up a regular schedule to revisit policies, metrics, and workflows. This routine will help compliance become second nature in your practice.
FAQs
What steps can clinics take to ensure their telehealth platform meets HIPAA compliance?
To maintain HIPAA compliance, clinics must focus on a few critical areas. First, they should use secure, encrypted communication channels to protect sensitive information. Second, implementing strict access controls is vital to ensure only authorized personnel can view patient data. Additionally, storing patient records in environments that meet HIPAA standards is non-negotiable. Regular staff training on privacy and security protocols is just as important to keep everyone informed and vigilant.
Platforms like Prospyr, which come equipped with built-in HIPAA-compliant security features, can make this process much easier. They provide a streamlined way to ensure your clinic adheres to all necessary regulations without added complexity.
How can I ensure a provider is properly licensed for telehealth services?
To verify a provider's license for telehealth services, begin by consulting the state medical board's database. This ensures their license is active and in good standing. It's also important to examine their credentials to confirm they meet the qualifications required for the services they offer. Keeping this information updated regularly is essential for staying compliant with telehealth reimbursement policies.
What’s the best way for a clinic to manage payer-specific telehealth requirements?
To stay on top of payer-specific telehealth requirements, start by building a detailed checklist for each payer. This should cover essentials like documentation guidelines, coding protocols, and billing policies. Make it a habit to review and update these checklists regularly to keep up with any changes.
A centralized system, such as Prospyr, can simplify this process by consolidating all requirements in one place. This not only keeps your team well-informed but also minimizes billing errors and ensures smoother reimbursements. It's a practical way to maintain compliance while boosting your clinic's efficiency.