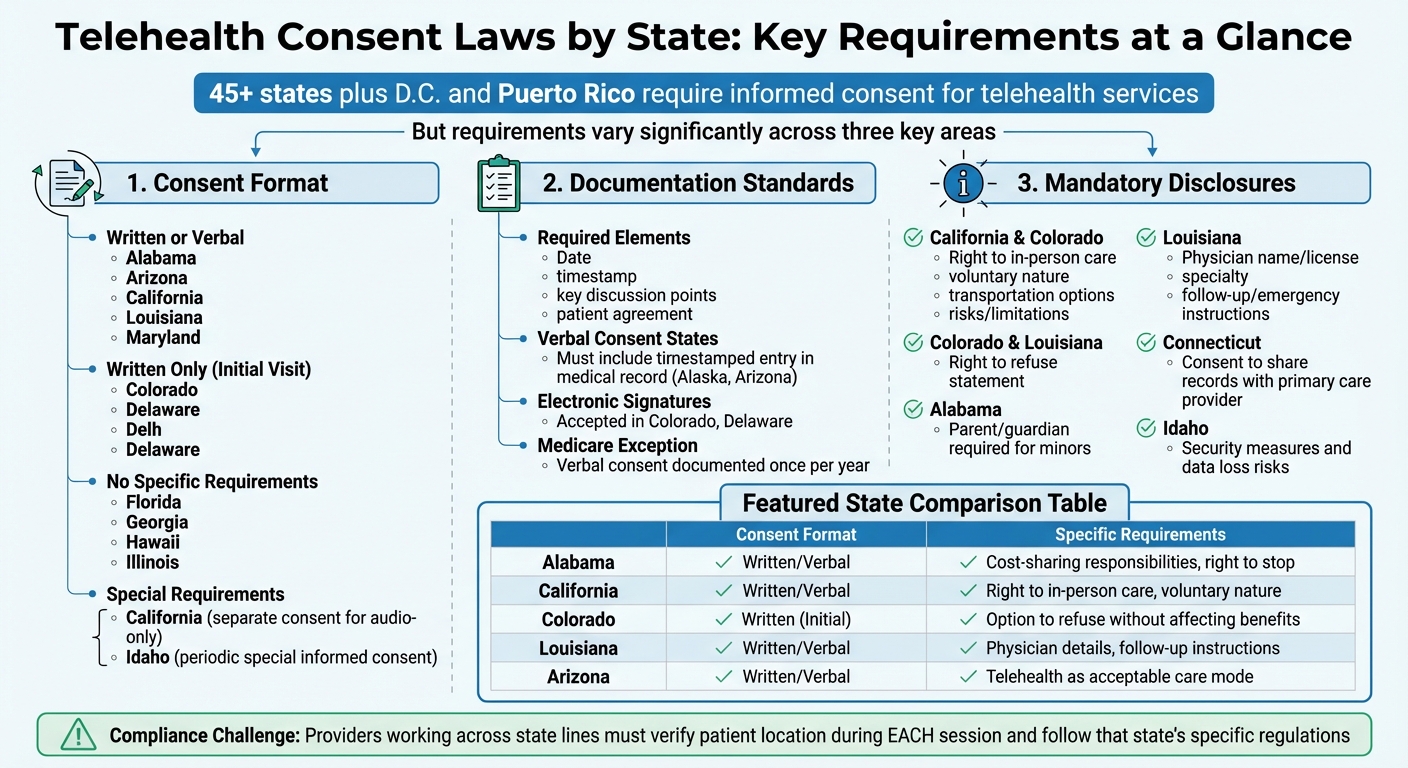
Telehealth consent laws in the U.S. vary significantly by state, creating challenges for healthcare providers. Most states (45 plus D.C. and Puerto Rico) require informed consent before telehealth services, but the specifics differ:
- Consent Format: Some states accept verbal or written consent, while others mandate written consent only.
- Documentation: Providers must record consent in the patient's medical record, often including details like session date and patient agreement.
- Disclosures: States may require providers to inform patients about risks, benefits, and the option for in-person care.
For providers working across state lines, compliance hinges on verifying the patient's location during each session and adhering to that state's regulations. Digital tools, like Prospyr, simplify this process by automating consent workflows and ensuring state-specific compliance.
| State | Consent Format | Key Disclosures |
|---|---|---|
| Alabama | Written or Verbal | Cost-sharing responsibilities; right to stop |
| California | Written or Verbal | Right to in-person care; telehealth is voluntary |
| Colorado | Written (Initial) | Option to refuse without affecting benefits |
| Louisiana | Written or Verbal | Physician details; follow-up care instructions |
| Arizona | Written or Verbal | Telehealth as an acceptable care mode |
Providers must stay updated on state laws and use standardized processes to ensure compliance while protecting patient rights.
Telehealth Consent Requirements by State: Format, Documentation, and Disclosures
1. State-Specific Telehealth Consent Requirements
State telehealth consent laws differ in three main areas: consent modality, documentation standards, and disclosure requirements. These variations are critical to understand, as failing to comply can result in penalties from state medical boards and other regulatory authorities.
Consent Modality
The way consent is obtained depends on the state. For example, Arizona, California, Colorado, and Maryland allow either verbal or written consent, provided it’s documented in the medical record. In California, providers must specifically note when a patient consents to audio-only telehealth interactions. Colorado, after the public health emergency, requires written consent for the first visit but allows verbal or written consent for follow-ups.
Some states enforce stricter rules. Delaware mandates written consent for most licensed professionals, while Idaho requires periodic "special informed consent" that includes details about security measures and potential risks of data loss. On the other hand, Florida, Georgia, Hawaii, and Illinois currently don’t have specific consent requirements for telehealth practitioners.
These varying consent methods directly influence how providers must document patient consent.
Documentation Standards
For states that allow verbal consent - such as Alaska or Arizona - providers must include a timestamped entry in the patient’s record to stay compliant. This entry should detail the date, key points of discussion, and the patient’s agreement.
California provides an exception for group practices: if the patient’s initial consent includes telehealth as an acceptable care option, individual providers within the group don’t need to re-document consent for future visits. For Medicare Communication Technology-Based Services, verbal consent only needs to be documented once per year.
Mandatory Disclosures
States also have specific requirements for what information must be disclosed to patients. California and Colorado are especially detailed, requiring providers to inform patients about their right to in-person care, the voluntary nature of telehealth, transportation options, and the risks or limitations of remote care. Louisiana adds additional requirements, such as disclosing the physician’s name, license number, specialty, and follow-up or emergency care instructions. Both Colorado and Louisiana also require a "right to refuse" statement, ensuring patients know they can choose in-person care without affecting future benefits.
Other states have unique requirements. For instance, Connecticut mandates that providers ask during the first interaction if patients consent to sharing their telehealth records with their primary care provider. In Alabama, a parent or legal guardian must attend telemedicine visits for minors who are under the age of medical consent.
| State | Consent Modality | Key Mandatory Disclosures |
|---|---|---|
| Alabama | Written or Verbal | Cost-sharing responsibilities; right to stop services at any time |
| California | Written or Verbal | Right to in-person care; voluntary nature; transportation options; risks/limitations |
| Colorado | Written (Initial); Verbal/Written (Subsequent) | Option to refuse without affecting future care; confidentiality protections |
| Louisiana | Written or Verbal | Physician name/license; specialty; follow-up/emergency care instructions |
| Arizona | Written or Verbal | Use of telehealth as an acceptable delivery mode; platform limitations |
These state-specific requirements underscore the importance of tailored digital intake tools from Prospyr to help providers stay compliant with diverse regulations.
sbb-itb-02f5876
2. Prospyr's Digital Consent Tools
Prospyr offers HIPAA-compliant digital forms designed to meet state-specific telehealth consent requirements, ensuring providers stay compliant no matter where they or their patients are located. The platform is flexible, accommodating both verbal and written consent workflows. It automatically adjusts based on the provider's license type and the patient's location. For example, a physical therapist in Delaware conducting remote sessions would need written consent, while a provider in Arizona has the option to choose between verbal or written consent - both of which are recorded in the patient’s medical record. Let’s break down how Prospyr handles consent through its modality, documentation, and mandatory disclosure features.
Consent Modality
Prospyr customizes consent workflows to align with the specific requirements of each state. The platform applies rules based on the provider’s license type, ensuring compliance with jurisdictional mandates. For example, the system adapts the consent process depending on whether verbal or written consent is needed, based on state-specific licensing guidelines.
Documentation Standards
Every consent record includes key details such as the session mode, identity verification, and the credentials of all participants. It also logs the physical locations of both the patient and provider during the session. In states like Colorado and Delaware, the platform supports electronic signatures and integrates these records directly into the patient’s medical file for seamless documentation.
Mandatory Disclosures
Prospyr goes beyond basic consent by automatically including state-required disclosures in its digital forms. These disclosures are tailored to the patient’s location. For instance:
- California: Forms highlight the right to in-person care, the voluntary nature of telehealth, and Medi-Cal transportation options for in-person visits.
- Colorado: Patients are informed that telehealth is optional, won’t affect their benefits, and maintains confidentiality protections.
- Idaho: Disclosures address the security measures in place and the risks of potential information loss due to technical issues.
- Connecticut: Patients can revoke their consent at any time, as required by state law.
This built-in functionality ensures that providers can manage telehealth consent requirements effortlessly while adhering to the unique regulations of each state. By automating these processes, Prospyr helps streamline compliance and improve the telehealth experience for both providers and patients.
3. Multi-State Compliance Best Practices
Managing telehealth across state lines requires a thoughtful and unified approach to consent. These practices work hand-in-hand with digital tools like Prospyr, which help simplify compliance with varying state regulations.
Consent Modality
A "highest common denominator" approach is a smart way to navigate multi-state compliance. By standardizing on written or electronic signatures for initial patient interactions, you can reduce the risk of non-compliance - even in states where verbal consent might suffice. Using HIPAA-compliant e-signature platforms adds an extra layer of security and consistency across jurisdictions. For example, California requires separate consent for audio-only services. Adding distinct checkboxes to your telehealth consent forms can make it easier to meet these specific requirements.
Once you’ve established a standardized consent process, the next step is to ensure clear and thorough documentation.
Documentation Standards
Every consent should be clearly documented in the EHR, including the date, key details, and confirmation of patient acknowledgment. A brief note confirming the patient’s understanding can further validate the consent. To avoid billing issues, integrate consent documentation directly into your EHR system, ensuring everything is recorded before a telehealth session takes place. For minors, it’s essential to confirm the identity of a parent or legal guardian, as per state laws.
With proper documentation in place, the focus shifts to meeting mandatory disclosure requirements.
Mandatory Disclosures
Create a universal disclosure form that reflects the strictest state requirements. This form should cover key elements like the right to in-person care, the voluntary nature of telehealth, potential risks, confidentiality protections, and access to medical records. Regularly auditing your consent procedures can help identify any gaps and ensure you stay compliant with changing regulations.
To make the process smoother, send consent forms through email or patient portals before appointments. This gives patients time to review the information and prepare any questions, helping to streamline the telehealth experience.
Pros and Cons
Weighing the benefits and challenges of various telehealth consent approaches highlights the complexities of ensuring compliance while maintaining efficiency. Here’s a closer look at the pros and cons of different methods:
| Approach | Pros | Cons |
|---|---|---|
| State-Specific Requirements | Helps patients understand telehealth risks, including technology failures and confidentiality concerns; enforces parity in care standards between telehealth and in-person visits (e.g., Alabama, Colorado); addresses specific risks tied to professions like social work, psychology, and veterinary care. | Creates a patchwork of regulations across 45+ states; manual tracking increases the chance of errors; documentation demands can overwhelm providers working in multiple states; non-compliance risks penalties from state medical boards. |
| Digital Consent Tools (Prospyr) | Automates compliance with multi-state variations, easing administrative workloads; offers clear audit trails for verification; integrates consent forms into telehealth systems; simplifies identity and location checks. | Involves upfront setup and possible subscription fees; requires patients to be comfortable with digital platforms; staff and less tech-savvy patients may need training. |
| Multi-State Best Practices | Standardized workflows simplify staff training; ensures a consistent patient experience across states; reduces the risk of missing key requirements by following a "highest common denominator" approach; builds patient trust and safeguards against malpractice claims and fines. | Can lead to lengthy consent forms that might overwhelm patients; a single "universal" form may overlook some niche state-specific disclosures; demands ongoing monitoring of legislative updates; Medicaid-specific nuances may complicate compliance. |
Finding the right balance between comprehensive patient protection and operational efficiency is key. Digital tools offer a practical solution, automating state-specific compliance while adapting to regulatory changes. Even in states with minimal requirements, adopting stricter standards can enhance legal protection and reflect a commitment to patient safety.
Conclusion
State telehealth consent laws present a complex landscape for aesthetic and wellness clinics, especially those operating across multiple states. These laws differ in their level of formality, required disclosures, and how often consent must be obtained, creating operational challenges.
"Noncompliance with telehealth legal requirements can result in civil, criminal, and administrative penalties from state medical boards and other regulatory bodies."
Prospyr helps navigate these challenges by automating state-specific consent requirements and maintaining clear audit trails. Its digital intake forms and HIPAA-compliant documentation ensure consent is captured and stored accurately in medical records, meeting the standards of nearly every state. This automation not only reduces administrative workload but also minimizes the risk of errors that could lead to penalties. These tools streamline compliance efforts while supporting effective multi-state operational strategies.
Standardizing consent workflows across states adds another layer of protection. Written consent processes with detailed disclosures - covering risks like technology failures, confidentiality limits, and the option for in-person care - help clinics maintain compliance, even in states with minimal requirements. Verifying patient identity and location during each session, thoroughly documenting consent, and staying updated on legislative changes are essential practices for building patient trust and ensuring regulatory adherence.
FAQs
What are the main differences in telehealth consent laws across states?
Telehealth consent laws differ from state to state, especially when it comes to how consent is obtained and recorded. In most cases, states require either verbal or written consent, but the exact procedures can vary. For instance, some states insist that providers confirm the patient’s identity and location, outline any limitations of telehealth services, or explain how protected health information (PHI) will be managed.
Additionally, certain states impose tighter restrictions on online prescribing, particularly for controlled substances, and may demand clear consent before sharing sensitive information. These variations underscore the need for healthcare providers to be well-versed in state-specific rules to stay compliant and safeguard patient rights.
What steps can healthcare providers take to comply with telehealth consent laws across different states?
Healthcare providers need to understand the specific telehealth consent laws in every state where they operate. These laws often address areas like licensure, informed consent, prescribing rules, and reimbursement guidelines. Keeping up with any updates to these rules is absolutely essential.
To stay compliant, providers can turn to state medical boards, legal experts, or policy resources for guidance. Leveraging tools such as digital consent forms and HIPAA-compliant platforms can also simplify the process while improving the overall experience for patients.
What tools can help ensure compliance with telehealth consent laws across different states?
Managing telehealth consent laws across different states can feel like navigating a maze, as each state has its own set of rules. To stay on top of these varying requirements, healthcare providers can turn to state-specific resources like legal summaries and regulatory guides. These tools break down the essentials, such as documentation and disclosure obligations, making it easier to align with compliance standards.
For an even smoother process, platforms like Prospyr offer practical solutions. With features like digital intake forms, HIPAA-compliant record management, and automated workflows, these tools not only simplify compliance but also improve operational efficiency. By streamlining these processes, providers can focus more on delivering quality patient care while staying up-to-date with telehealth regulations.



