Timely filing deadlines are the strict time limits insurers set for submitting claims after services are provided. Missing these deadlines leads to automatic claim denials and financial losses, as clinics typically cannot bill patients for late claims. Medicare allows 12 months from the date of service, while commercial insurers like UnitedHealthcare or Cigna often enforce deadlines of 90–180 days. Medicaid deadlines vary by state, ranging from 90 days to 12 months.
Key points to remember:
- Medicare: 12 months from the date of service.
- Commercial Insurance: 90–180 days, with some like Magellan Health requiring submission within 60 days.
- Medicaid: State-specific deadlines (e.g., Texas: 95 days; Florida: 12 months).
- Medicare Advantage: Typically 90–180 days, shorter than Original Medicare.
To avoid revenue loss:
- Submit claims promptly, ideally daily.
- Use software for deadline tracking and alerts.
- Maintain a reference guide for payer-specific deadlines.
Late claims are rarely appealable, especially for Medicare. Commercial insurers may allow appeals but often require proof of timely submission. Efficient systems and proactive management are essential to protect your clinic's revenue.
Filing Deadlines by Payer Type
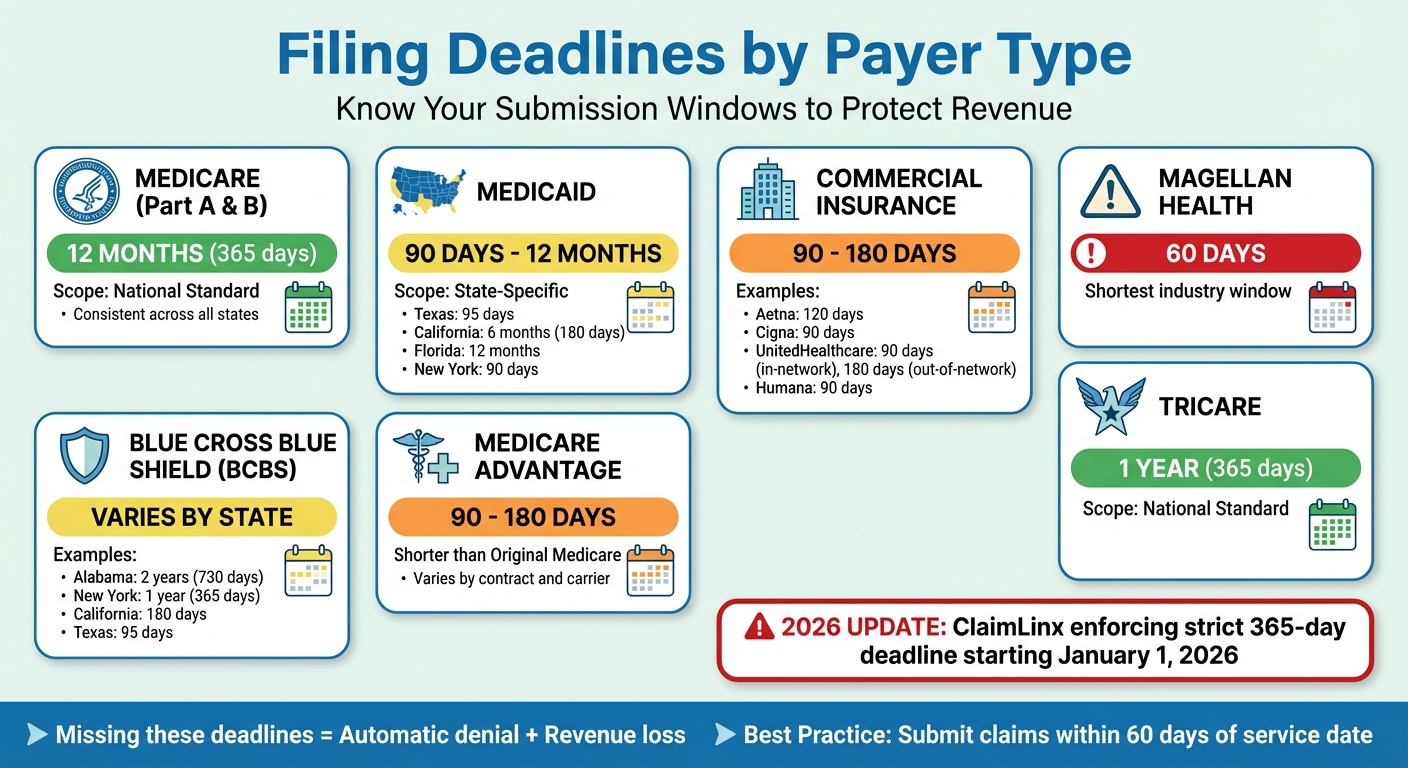
Healthcare Insurance Filing Deadlines by Payer Type 2024-2026
Medicare, Medicaid, and Commercial Insurance Deadlines
Knowing the filing deadlines for different payer types is crucial for safeguarding your clinic's revenue. Utilizing advanced revenue analytics can help identify patterns in these denials before they impact your bottom line. Medicare has a consistent 12-month (365-day) deadline for submitting claims, whether they fall under Part A (institutional) or Part B (professional) services.
Medicaid deadlines, however, are determined by individual states and can vary widely, from as little as 90 days to as much as 12 months. For example, Texas Medicaid requires claims to be submitted within 95 days, while Florida Medicaid permits up to 12 months. This variability means Medicaid billing demands a tailored, state-specific approach, often starting with digital intake to ensure all required state data is captured upfront.
Commercial insurance providers generally require claims submissions within 90 to 180 days. Aetna, for instance, typically allows 120 days, while both Cigna and UnitedHealthcare require claims to be filed within 90 days for in-network providers and up to 180 days for out-of-network providers. Magellan Health stands out with one of the shortest filing windows in the industry - just 60 days.
Medicare Advantage plans, though part of the Medicare system, often have shorter filing limits than the 12 months allowed under Original Medicare. These plans usually operate within a 90- to 180-day timeframe, which can catch clinics off guard, especially those transitioning from traditional Medicare.
Next, let’s look at how state-specific regulations further influence these deadlines.
How State Rules Affect Filing Deadlines
State regulations add another layer of complexity to filing deadlines, particularly for Medicaid, Workers’ Compensation, and state-regulated exchange plans. While major commercial insurers like Aetna, Cigna, and UnitedHealthcare tend to follow national filing standards, individual provider contracts can override these policies.
Blue Cross Blue Shield (BCBS) is a unique challenge for clinics operating in multiple states. BCBS functions as a network of independent companies across states, leading to varied filing limits. For example, BCBS Alabama allows a generous 2-year filing window, while BCBS Texas limits claims to just 95 days. Other states fall somewhere in between, such as California with a 180-day deadline and New York with a 1-year limit.
Medicaid filing deadlines also differ significantly by state. New York Medicaid generally requires claims within 90 days, while states like Virginia and Florida extend this to 12 months. California Medicaid sits in the middle, with a 6-month window. Additionally, for secondary or tertiary claims, the filing deadline usually starts from the primary payer’s determination date (EOB date) rather than the original service date.
Filing Deadline Comparison Table
Here’s a quick comparison of filing deadlines across payer types:
| Payer Type | Standard Filing Limit | State-Specific Examples |
|---|---|---|
| Medicare (Part A & B) | 12 Months | National Standard |
| Medicaid | 90 Days – 1 Year | Texas: 95 Days; Florida: 12 Months; California: 6 Months |
| Commercial | 90 – 180 Days | Aetna: 120 Days; Cigna: 90 Days; Humana: 90 Days |
| BCBS | Varies by State | New York: 1 Year; California: 180 Days; Texas: 95 Days; Alabama: 2 Years |
| Medicare Advantage | 90 – 180 Days | Varies by contract and carrier |
| TRICARE | 1 Year | National Standard |
| Magellan Health | 60 Days | National Standard |
sbb-itb-02f5876
2026 Regulatory Updates
ClaimLinx One-Year Filing Rule
Starting January 1, 2026, ClaimLinx will enforce a strict one-year filing deadline - 365 days from the date of service - for all claim types. Claims submitted after this period will be denied as untimely. Depending on the terms of the patient's contract, the financial responsibility may shift to the patient. However, exceptions will be made for cases of documented medical incapacity or extraordinary circumstances.
ClaimLinx shared their reasoning behind this policy change:
"Moving to a one-year standard ensures we remain consistent and in step with industry expectations. It also helps reduce delays, streamline processing, and make the claims experience smoother for everyone involved."
To prevent delays, clinics are encouraged to submit claims promptly after services are rendered. Using electronic data interchange (EDI) or payer portals can expedite the process and provide instant confirmation of receipt. This change reflects a broader trend within the healthcare industry toward more uniform filing deadlines.
Industry Movement Toward Standard Deadlines
ClaimLinx's new policy aligns with a growing industry trend toward standardized filing deadlines. Many major medical carriers now enforce deadlines ranging from 90 days to 12 months. Meanwhile, Medicare's established 12-month deadline remains unchanged.
A notable update came from the Centers for Medicare & Medicaid Services (CMS) in October 2024 with CMS Change Request 12909. This update eliminated the timely filing period for claim adjustments, allowing clinics to submit corrected claims beyond the 12-month window, provided the original claim was filed on time. These developments emphasize the importance of implementing effective deadline-tracking systems to ensure timely submissions and optimize revenue collection.
How to Track and Meet Filing Deadlines
Documentation and Submission Best Practices
Start by verifying insurance eligibility during patient check-in. Use real-time EDI verification tools to capture accurate insurance details, including IDs and effective coverage dates. This simple step helps prevent errors at the front end that could delay claims later. Once services are provided, make sure providers promptly close and sign charts.
Submitting claims daily can reduce denial rates by up to 20%. This practice avoids backlogs and ensures claims are processed while you still have maximum filing time. Keep in mind that clearinghouse rejections don’t stop the filing clock, so it’s crucial to monitor these daily to confirm claims are successfully reaching payers. Additionally, systematically archive 277CA reports to verify that claims have been received by the payer before the deadline.
These steps lay the groundwork for using technology to make deadline management even more efficient.
Using Software to Manage Deadlines
Practice management software can take the headache out of tracking deadlines. Platforms like Prospyr offer task management tools that automate workflows, flagging claims as they approach critical deadlines. Real-time analytics provide visibility into the aging of claims, helping staff prioritize submissions before time runs out.
Set up your system to send alerts at key intervals: Yellow Flags when 75% of the deadline has passed, Red Flags at 85%, and Critical Alerts at 90%. Built-in claim scrubbing tools are also invaluable - they catch issues like missing data, incorrect CPT/ICD codes, or formatting errors before the claim is submitted. This can prevent rejections that eat into your filing window. Aim for a success rate of 98% or higher for claims filed within your internal deadlines. If your success rate falls below this, it’s a sign your workflow needs adjustment.
Creating Internal Deadline Systems
While software is a powerful tool, internal systems are equally important for ensuring timely submissions. Set internal deadlines that are well ahead of payer limits. For example, aim to submit claims within 60 days if the payer’s deadline is 90 days. This buffer is critical since reworking a denied claim can cost between $25 and $118.
Assign a dedicated "Expiring Claims Champion" to pull weekly aging reports and focus on resolving claims nearing their deadlines. This role ensures there’s always someone accountable for keeping claims on track. Additionally, maintain a master reference document that lists all contracted payers' deadlines, how they calculate them (e.g., from the service date or primary payment date), and whether they extend deadlines for weekends or holidays. Most commercial carriers count calendar days without offering extensions for weekends, meaning claims due on a weekend must be submitted by the Friday before.
Handling Denials and Filing Appeals
How to Prevent Late Filing Denials
Preventing late filing denials starts with accuracy at the very beginning of the process. At the front desk, verify insurance eligibility during the patient's visit and ensure the correct plan type is selected. For instance, Medicare Advantage operates differently from traditional Medicare, and Managed Medicaid has its own set of rules compared to fee-for-service Medicaid. A small mistake here - like sending a claim to the wrong payer - can waste critical filing time. Additionally, confirm that providers are fully credentialed with each payer. If they aren’t, you might only discover the issue after the claim is denied, often too late to fix within the filing window.
Using aging reports effectively can make a big difference. Run these reports weekly and focus on claims that are 30 to 60 days old. This gives you a buffer to address any problems before the filing deadline. Also, consider submitting claims daily instead of batching them weekly - this simple shift can reduce denial rates by nearly 20% and allows more time to identify and correct errors.
Even with these precautions, some claims may still face denials. That’s when the appeal process comes into play.
The Appeal Process for Late Claims
For Medicare claims denied due to late filing, appeals are not an option. According to CMS guidelines, these denials don’t qualify as an "initial determination", which means standard appeal rights don’t apply. The CMS Internet-Only Manual clarifies this:
"When a claim is denied for having been filed after the timely filing period, such denial does not constitute an 'initial determination.' As such, the determination that a claim was not filed timely is not subject to appeal."
In these cases, your only recourse is to request a waiver or exception. To do this, use a Part B Reopening Request Form rather than a standard redetermination form. Your submission should include a detailed explanation of why the claim was filed late, supported by relevant documentation. Acceptable reasons might include administrative errors by Medicare, retroactive Medicare entitlement, or backdated coverage. If you’re submitting the request by fax, always save the confirmation page as proof of timely submission.
When dealing with commercial payers, the rules vary. Most allow a 90- to 180-day window from the denial date to file an appeal. Be sure to include proof of timely submission, such as 277CA reports showing the claim reached the payer before the deadline. However, keep in mind that if your appeal is rejected, you typically cannot bill the patient for the remaining balance - you’ll bear the financial loss.
Key Takeaways
Staying on top of timely filing is crucial for safeguarding your revenue cycle. Claims denials cost hospitals billions every year, with timely filing consistently ranking among the top five reasons for these losses. For smaller practices, the stakes are just as high. Missing out on 20 claims per week, valued at $200 each, can add up to nearly $48,000 in lost revenue annually.
"Timely filing isn't just a checkbox - it's one of the most overlooked yet costly pitfalls in revenue cycle management". - Manish Jain, MBW RCM
Automation can be a game changer. It cuts down administrative tasks by 42%, speeds up reimbursements by 42%, and reduces average accounts receivable days by 34%. Practices that switch from weekly to daily claim submissions often experience a nearly 20% drop in denial rates. Setting internal deadlines 15–30 days ahead of payer cut-offs allows room to fix errors before they escalate into costly problems.
The numbers speak volumes - 20% of claims are initially denied, and a staggering 60% of those are never resubmitted. Reworking a claim costs anywhere from $25 to $118 on average, and handling a denied claim takes two to four times more staff time compared to processing a clean submission. Smarter deadline management is the answer.
This is where Prospyr's practice management platform steps in. It automates deadline tracking, integrates billing tools, and provides real-time alerts alongside claim scrubbing features. By identifying errors before submission and keeping tabs on claim statuses automatically, it safeguards your revenue while reducing administrative strain. The HIPAA-compliant system works seamlessly with your existing processes, ensuring claims flow smoothly from service to payment.
FAQs
What is considered the “timely filing” date for my claim?
The "timely filing" date refers to the deadline a payer sets for submitting your claim. For Medicare, Medicaid, and many insurance plans, this deadline is usually one calendar year from the date of service. That said, deadlines can differ depending on the payer, so it’s crucial to check their specific policies to prevent claim denials.
Do corrected claims or claim adjustments have the same deadline?
Corrected claims and claim adjustments follow different submission deadlines. For adjustments, you have 12 months from the processing date to submit them. On the other hand, original claims typically need to be filed within 12 months from the date of service. It's crucial to monitor these timeframes closely to ensure you meet the deadlines.
What proof should I keep to win a timely filing appeal?
To ensure you can back up a timely filing appeal, always retain electronic submission receipts and clearinghouse reports. These records are crucial for proving that your claims were submitted within the designated timeframe.


